About a year ago, in a context I’ve now forgotten, one of our classmates, Selim Arcasoy, mentioned the fat paradox during a class discussion. He explained, “Overweight people may have a lower mortality rate.” It momentarily registered in my brain, but I quickly filed it away as “statistical noise.” Since then, I heard about it again in a conversation about how the public health community sometimes ignores data, especially if it contradicts our popular conventions (like “being overweight is bad”, for example). The issue raises questions about interpretation of data that conflicts with widely held beliefs and how such findings may not impact practice. To better understand the fat paradox, I decided to go to the source…
Flegal and team, from the National Center for Health Statistics, published a meta-analysis in JAMA in 2013 entitled, “Association of All-Cause Mortality with Overweight and Obesity Using Standard Body Mass Index Categories.”  They found that overweight participants had a lower hazard ratio for all-cause mortality compared with normal weight participants. To come to this conclusion, Flegal’s team reviewed 97 studies that included more than 2.88 million participants and over 270,000 deaths conducted in numerous countries (mostly the U.S. and Europe) through September 2012. They included studies that were adjusted for age, sex, and smoking but, interestingly, not for diseases that are part of the “obesity mortality pathway” such as hypertension because this would lead to “over-adjustment”. The meta-analysis found that relative to those with normal weight, grade 1 obese participants (see definitions below) had a similar mortality hazard ratio (HR) while those who were grade 2 or 3 obese had an increased mortality HR. In contrast, those who were overweight had a lower mortality HR (0.94, 95% CI, 0.91 – 0.96) compared with those who were normal weight.
They found that overweight participants had a lower hazard ratio for all-cause mortality compared with normal weight participants. To come to this conclusion, Flegal’s team reviewed 97 studies that included more than 2.88 million participants and over 270,000 deaths conducted in numerous countries (mostly the U.S. and Europe) through September 2012. They included studies that were adjusted for age, sex, and smoking but, interestingly, not for diseases that are part of the “obesity mortality pathway” such as hypertension because this would lead to “over-adjustment”. The meta-analysis found that relative to those with normal weight, grade 1 obese participants (see definitions below) had a similar mortality hazard ratio (HR) while those who were grade 2 or 3 obese had an increased mortality HR. In contrast, those who were overweight had a lower mortality HR (0.94, 95% CI, 0.91 – 0.96) compared with those who were normal weight.
Standard Body Mass Index (BMI) Categories
Underweight: < 18.5
Normal weight: 18.5 – < 25
Overweight: 25 – < 30
Obesity grade 1: 30 – < 35
Obesity grade 2: 35 – < 40
Obesity grade 3: < 40
In case you’re curious about your BMI, you can check here: http://www.nhlbi.nih.gov/guidelines/obesity/bmi_tbl.pdf
One of the major criticisms of the analysis is that the normal weight group contained people who may have had mortality risks including heavy smoking, advanced age, serious illness or infectious diseases that weren’t adequately controlled for and therefore served as confounders. Critics say that the researchers should have removed smokers altogether, though Flegal argues that this would eliminate a substantial amount of key data. Last, among over-weight patients, results were similar in adjusted and over-adjusted groups, thus demonstrating that diseases like hypertension were less likely to be confounders.
When looking at subgroups, the relationship between obesity and increased mortality decreases as people age. In a paper by Virginia Huges published in Nature in 2013, a U-shaped curve describes the relationship between mortality and weight among older populations. 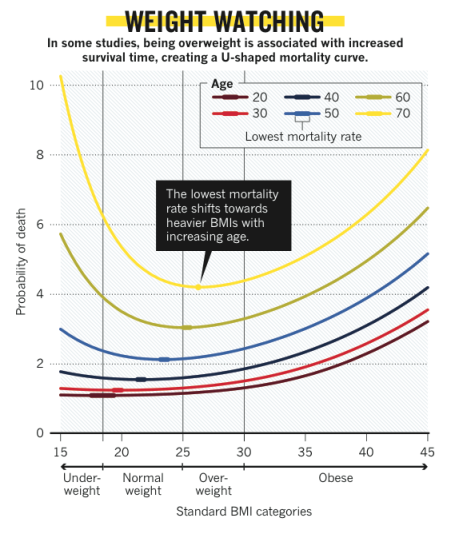 Interestingly, this curve was originally described by the National Institute on Aging based on actuarial tables decades ago. They found that the lowest mortality rate for 30 year-olds was among those with a BMI of ~20 but for 70 year-olds, the rate was lowest among those with a BMI of ~27.
Interestingly, this curve was originally described by the National Institute on Aging based on actuarial tables decades ago. They found that the lowest mortality rate for 30 year-olds was among those with a BMI of ~20 but for 70 year-olds, the rate was lowest among those with a BMI of ~27.
What could explain all this? One theory is that among people with serious diseases (e.g. diabetes or heart disease), those who are overweight have more energy reserves to fight off illness. Others think that excess weight might help protect people during trauma and falls, particularly among the elderly. Still others believe that the underlying issue lies in what we are measuring…
What got David Lederer, a pulmonologist and lung transplant doctor at Columbia University Medical Center, interested in these weighty issues? He noticed a trend. Patients with a BMI greater than 30 were being turned down for new lungs.  Why? Because there was a smattering of smallish, single-center trials that consistently showed the same trend – obese patients had high rates of early mortality after getting new lungs. David wondered why we were looking at such small studies so he tapped into the United Network for Organ Sharing (UNOS) database to learn more. After analyzing this immense data set and controlling for other variables, David still “couldn’t make the association go away” and found that obese patients had a 10-70% increase in mortality in the first year post-transplant (the wide range is partly due to co-morbidities).
Why? Because there was a smattering of smallish, single-center trials that consistently showed the same trend – obese patients had high rates of early mortality after getting new lungs. David wondered why we were looking at such small studies so he tapped into the United Network for Organ Sharing (UNOS) database to learn more. After analyzing this immense data set and controlling for other variables, David still “couldn’t make the association go away” and found that obese patients had a 10-70% increase in mortality in the first year post-transplant (the wide range is partly due to co-morbidities).
Though he doesn’t consider himself an “obesity person” he forged ahead to better understand what was behind all this by assembling a multi-site team of scientists and clinicians. They’re now embarking on a prospective study looking beyond BMI to better understand how obesity is related to outcomes in lung transplant patients. Specifically, they’re investigating relationships among imaging, inflammatory mediators in fat tissue around lungs, and biomarkers in the blood like leptin (which regulates appetite), adiponecin (a protective hormone), and ghrelin (which stimulates hunger)…believe me, there are more… After better understanding these relationships, the idea is to find a variable more specific than BMI to predict lung transplant outcomes.
So how does this all relate to the original question: do overweight people have a decrease in mortality and if so why? David thinks it’s an interesting question, but suggests we should step back and define terms. “BMI is wonderfully useful at the population level. But on the individual level it’s less clear.” BMI is just one method of measuring body composition. He shows me a slide from a presentation listing others, including hydrometry, CT/MRI, ultrasound, and even dual-energy x-ray absorptiometry (or DXA-scan) – yes, the thing that measures bone density turns out to be a safe way to measure body fat. Preliminary findings of his study indicate that BMI does not correlate well with total body fat in lung transplant patients. It lacks specificity partly because of fluid and muscle mass. Remember, body builders like Schwarzenegger (back in the day) would be classified as morbidly obese because of weight. Whether it’s from muscle, fat, or fluid, BMI doesn’t know. Last, David wonders if the “normal weight” patients in the Flegal meta-analysis did worse because they might be actually losing weight (unintentional weight loss is a marker of disease), which is why a longitudinal study might be of use. He does agree, however, that having a little fat can be protective before a big surgery or during falls or trauma. His explanation of the limitations of BMI shed light on the issue and we look forward to reading the findings of his study.
After talking to David Lederer, I began to wonder if misclassification is the root of the controversy. While I think it may be contributing, I don’t think it’s the full answer. Part of the problem is that it’s a very difficult thing to study. We simply cannot replicate a single individual, keep everything constant (in terms of disease, exercise, social interaction) and give one double the calories (of the same food) to see what happens. We have to rely on studies in spite of their limitations. As a result, people combine study findings like Flegal’s with their own personal experiences to come up with a perspective on reality. Perhaps we should focus on what we do know: that a diet rich in fruits and vegetables, low in sugar and processed foods plus a lifestyle filled with exercise and activity prolongs life. These ideas are consistent with the work of Steven Blair (exercise scientist with University of South Carolina’s school of public health) who writes that focusing on the right behaviors (such as diet and exercise) leads to health irrespective of weight. He recommends at least 30 minutes of moderate intensity exercise on five or more days per week. I think his work reorients our focus – not solely on weight – but what’s beyond the weight. If eating kale for dinner decreases one’s blood glucose and walking in the park increases life expectancy, shouldn’t we give proper accolades to the kale – and to attractive walking shoes – as opposed to putting it all into one number?
Special thanks to Catherine Dentinger for edits and contributions on this blog post!
